By Dr.Manvir Bhatia & Ananya-17th Feb 2023, Health and Sleep
Obstructive Sleep Apnoea(OSA) is a condition characterized by frequent, loud snoring, periods of breathlessness during sleep, and excessive daytime sleepiness. Obesity and craniofacial structures are major contributors to it. It affects around 1-4% of the general population and about 25-30% of obese individuals.
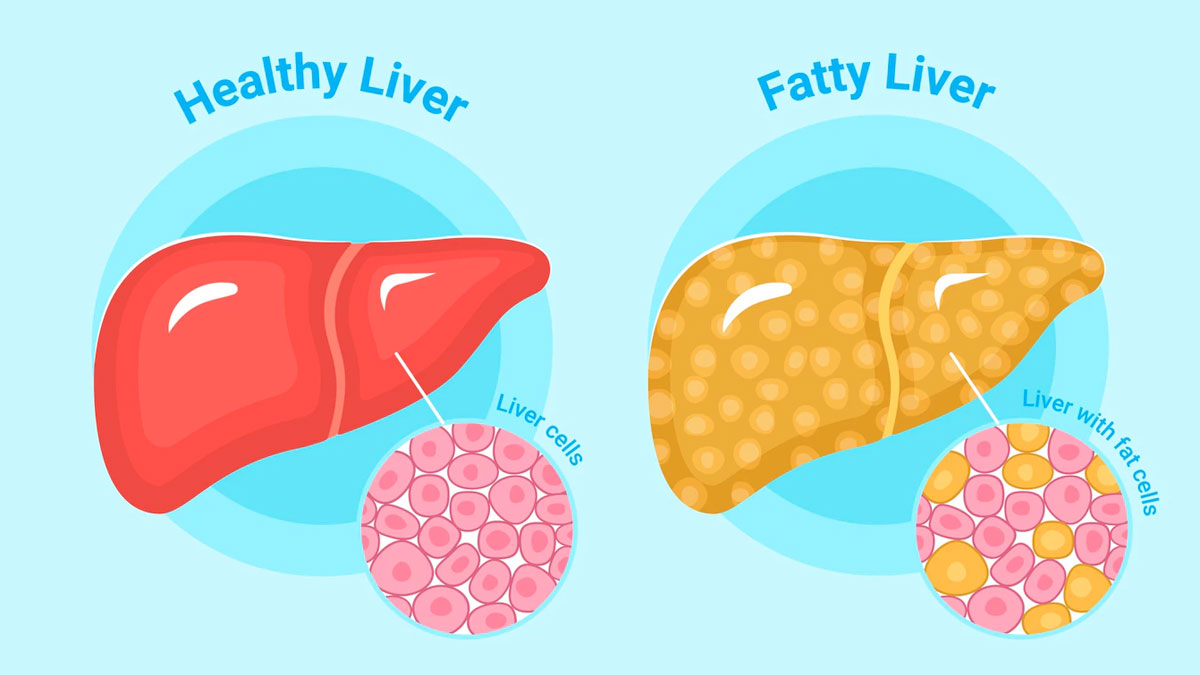
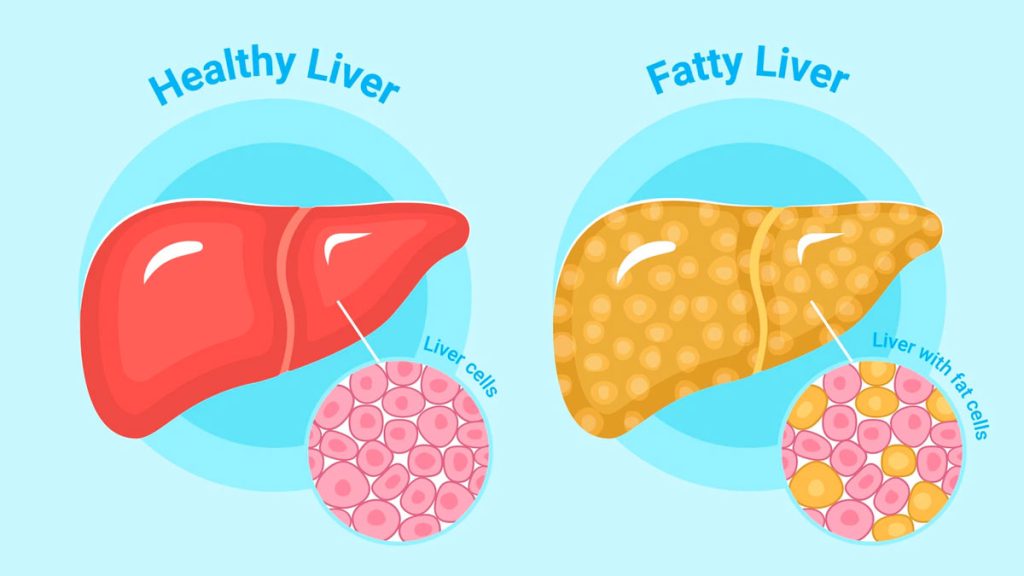
Nonalcoholic fatty liver disease(NAFLD) comprises a wide spectrum of liver damage. This includes steatosis, steatohepatitis, advanced fibrosis, and cirrhosis. It is characterized by the presence of more than 5% of fat in the liver when the consumption of alcohol is less than 10g per day. It is an important health concern across the globe and is strongly associated with insulin resistance, type 2 diabetes, obesity, and hyperlipidemia. It is also a cause of great concern as it can silently progress to cirrhosis, portal hypertension, and death in early adulthood because of damaged liver. OSA is also considered a potential cause of NAFLD because of its association with insulin resistance and hyperlipidemia. Also, hypoxia (which occurs in OSA) is considered to be a factor that aggravates OSA. OSA has been found to play a role in the progression of NAFLD to non-alcoholic steatohepatitis.
It has been established that obese people are always at a higher risk of insulin resistance(IR) and type 2 diabetes mellitus(T2DM). A similar association has been observed between OSA and insulin resistance. IR leads to excessive accumulation of triglycerides in the cells of the liver, which is the hallmark of NAFLD.
In a study by Vgontzas et al., it was observed that there was a marked increase in insulin resistance in obese individuals with OSA as compared to non apneic obese individuals. These OSA patients had higher levels of visceral fat as compared to the obese controls. Hence, sleep-disordered breathing has a positive correlation with visceral fat.
There are various studies that have shown that OSA is a trigger for inflammation. NF-κB is the transcription factor associated with inflammatory pathways and to some extent can also affect insulin sensitivity. The levels of NF-κB increase in cases of OSA, obesity, and metabolic syndrome. The levels of TNF-α and IL1, mediators of inflammatory and immune responses, also follow a similar pattern.
Adipocytes produce a cytokine known as adiponectin. A reduction in the levels of adiponectin leads to insulin resistance in the case of obese individuals. A decrease in its levels is also associated with NAFLD. Hypoxia and TNF-⍺ reduce the adiponectin expression in adipocytes and can thereby lead to NAFLD.
There are five established criteria for metabolic syndrome. These include the increased circumference of the waist, high levels of triglycerides, reduced amounts of high-density lipoprotein (HDL), high blood pressure, and elevated fasting glucose levels. NAFLD is considered the hepatic part of metabolic syndrome. According to a study by Vgontzas et al., obese sleep apnea patients have a greater amount of visceral fat as compared to the obese controls. Also, there is a positive correlation between sleep-disordered breathing and visceral fat. Hence, this suggests that OSA is a part of metabolic syndrome. OSA is also associated with an increased risk of cardiovascular diseases(CVD) be it in presence of the metabolic syndrome. However, the presence of OSA along with metabolic syndrome increases the incidence of CVDs. This complex relationship between OSA, metabolic syndrome, and NAFLD indicates that in the case of a person suffering from any CVD, it is very important to diagnose and treat these three mentioned conditions.
NAFLD is also associated with dyslipidemia. Studies by Tomasova et al., in rats, demonstrate that acute hypoxia increases the levels of LDL cholesterol (bad cholesterol). Repeated exposure to hypobaric hypoxia leads to a decrease in levels of good cholesterol(HDL) and an increase in that bad cholesterol(LDL, VLDL), fatty acids, and chylomicron. Hence, this indicates that hypoxia(a characteristic of OSA) might lead to an increase in the levels of lipids in the plasma and the liver which can further precipitate fatty liver.
We conclude that obstructive sleep apnoea and fatty liver disorders(specifically NAFLD) are deeply interlinked not only with each other, but a number of conditions like cardiovascular disorders, obesity, insulin resistance, etc. Therefore, treatment of either of these conditions is dependent on the diagnosis and management of the other. For example, if a person is diagnosed with NAFLD, she should be also screened for OSA and vice versa. A regular good sleep routine, sufficient sleep, regular exercise and meditation, family work-life balance, healthy diet, etc. are a few efforts that an individual can put in to avoid the conditions of OSA and NAFLD. Also, consultation with an experienced professional becomes very important for the good management of these conditions.
References:
Ahmed, M. H., & Byrne, C. D. (2010). Obstructive sleep apnea syndrome and fatty liver: association or causal link? World journal of gastroenterology, 16(34), 4243–4252. https://doi.org/10.3748/wjg.v16.i34.4243
Tomásová, H., Lisý, V., Trojan, S., & Stastný, F. (1987). Effect of short-term or intermittent hypobaric hypoxia on plasma lipids in young rats. Physiologia Bohemoslovaca, 36(4), 361–364.
Vgontzas, A. N., Papanicolaou, D. A., Bixler, E. O., Hopper, K., Lotsikas, A., Lin, H. M., Kales, A., & Chrousos, G. P. (2000). Sleep apnea and daytime sleepiness and fatigue: relation to visceral obesity, insulin resistance, and hypercytokinemia. The Journal of clinical endocrinology and metabolism, 85(3), 1151–1158. https://doi.org/10.1210/jcem.85.3.6484
For any issues related to sleep and neurology visit-www.neurologysleepcentre.com