Written by Aisha, Reviewed by Dr. Manvir Bhatia, 1/12/2025
Sleep studies, such as Polysomnography (PSG), are essential for diagnosing sleep disorders such as sleep apnea and periodic limb movement disorder. However, for some patients, it’s equally important to assess lung function before undergoing a PSG test. Understanding when and why a lung function test (spirometry or pulmonary function test) is needed can help ensure accurate sleep study results and safer testing.
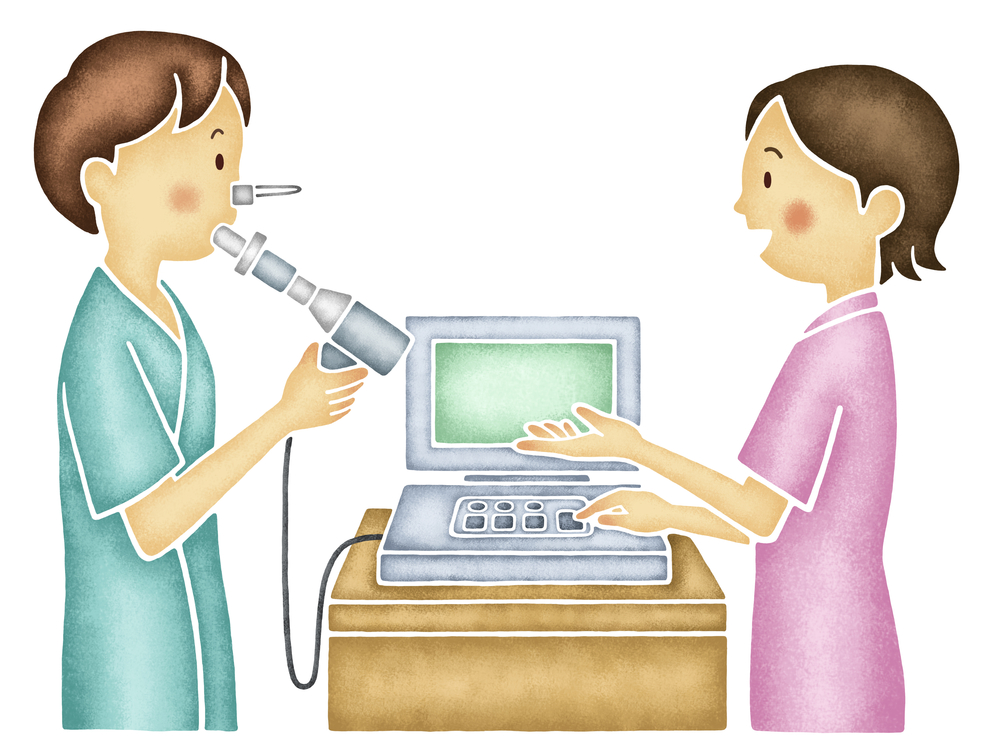
What is a pulmonary Function Test (PFT)?
A Pulmonary Function Test (PFT) — also known as a Lung Function Test — is a simple, non-invasive test that measures how well your lungs work.
It checks:
- How much air can you inhale and exhale?
- How quickly can you breathe out?
- How efficiently do your lungs transfer oxygen into your blood?
The most common part of a PFT is spirometry, where you’ll be asked to take a deep breath and blow forcefully into a mouthpiece connected to a computer.
It’s quick, safe, and usually takes 10–15 minutes.
Why Lung Function Testing May Be Needed Before a PSG
Sleep and breathing are closely connected. If your lungs aren’t working properly, it can affect your sleep quality and oxygen levels during sleep. Performing a Pulmonary function test before a PSG helps identify or rule out underlying respiratory conditions that may influence your sleep results.
Here are a few scenarios where a PFT before PSG is recommended:
1. When You Have Chronic Respiratory Symptoms
If you experience chronic cough, wheezing, shortness of breath, or chest tightness, your doctor may order a lung function test first. These symptoms may indicate asthma, COPD, or restrictive lung disease, which can worsen sleep-related breathing disorders.
2. In Patients with Known Lung Disease
Patients already diagnosed with conditions like asthma, COPD, interstitial lung disease, or post-COVID lung issues should undergo LFT before a PSG. This ensures your sleep data is interpreted correctly in the context of your lung function.
3. When Sleep Apnea Is Suspected in a Respiratory Patient
If you have both respiratory problems and sleep-related symptoms (such as snoring, morning headaches, or daytime fatigue), performing a lung function test first helps determine the contribution of lung disease to the symptoms.
4. For Pre-CPAP Assessment
In cases where CPAP (Continuous Positive Airway Pressure) therapy is anticipated after PSG, lung function testing helps in optimizing pressure settings and ensuring that your lungs can tolerate positive pressure effectively.
5. Before Evaluating Hypoventilation or Oxygen Desaturation
If you have low oxygen levels at night, your doctor may request an PFT to assess your lung’s capacity and exclude pulmonary causes of hypoventilation before attributing it solely to sleep apnea.
How the Two Tests Complement Each Other
A Pulmonary Function Test (PFT) and a Polysomnography (PSG or Sleep Study) serve different but closely related purposes in understanding your respiratory and sleep health. When performed together, they give a complete and accurate assessment of how your lungs and breathing behave during both daytime and sleep.
1. Pulmonary Function Test (PFT) – Daytime Assessment
A Pulmonary Function Test evaluates how well your lungs work while you are awake. It measures:
- Airflow and lung volume — how much air you can inhale and exhale.
- Gas exchange efficiency — how effectively your lungs deliver oxygen to your blood.
- Airway resistance — how easily air moves through your respiratory passages.
This helps detect or monitor conditions like asthma, COPD, restrictive lung diseases, or other respiratory limitations that may affect your breathing even before bedtime.
2. Polysomnography (PSG) – Nighttime Evaluation
A Sleep Study records your breathing, oxygen saturation, brain waves, heart rate, and body movements throughout the night. It identifies:
- Sleep apnea or hypopnea episodes
- Drops in oxygen levels (desaturation)
- Disrupted sleep patterns or snoring-related issues
PSG focuses on how your breathing patterns and oxygen levels behave during sleep, when muscles relax, and breathing control changes.
3. Why They Work Best Together
When both tests are done, your doctor can connect the dots between daytime lung performance and nighttime breathing disturbances.
Together, they help to:
- Determine whether sleep apnea is linked to an existing lung condition.
- Identify if reduced lung capacity contributes to low oxygen levels during sleep.
- Personalize treatment—such as CPAP/APAP therapy—based on both your lung function and sleep-related breathing patterns.
- Monitor the effectiveness of ongoing treatment to ensure optimal respiratory and sleep health.
Key Takeaway
A pulmonary function test before a PSG isn’t mandatory for everyone — but it’s highly beneficial for those with breathing issues, lung conditions, or unexplained oxygen drops during sleep. It ensures a safe, comprehensive, and personalized approach to diagnosing sleep-related breathing disorders.