Written By Arshad, Reviewed by Dr. Manvir Bhatia-18/04/2025
A Simple, Clear Guide for You and Your Loved Ones
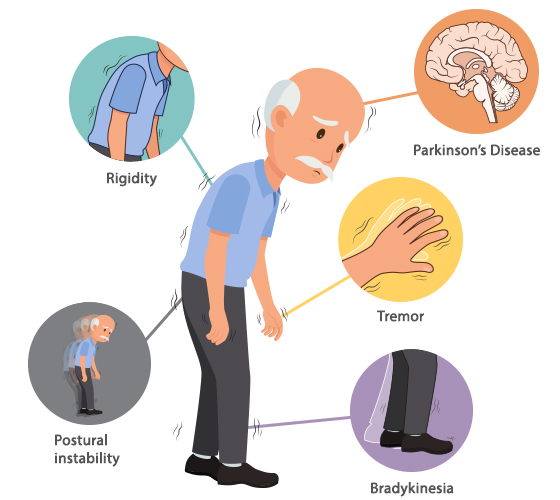
Parkinson’s Disease (PD) is a progressive brain disorder that affects movement, often starting subtly and getting more noticeable over time. You might associate it with shaky hands, stiffness, or slower walking, but how exactly do doctors figure out that it’s Parkinson’s?
Let’s walk you through the process in simple, everyday language.
Diagnosis Begins with Observation — Not a Blood Test
Unlike many conditions, no single test can definitively say, “This is Parkinson’s.” Instead, neurologists — doctors specializing in the brain and nerves — rely on a detailed understanding of your symptoms and what they observe during a physical exam.
They’ll ask you about things like:
- How has your movement changed
- Whether you’re having trouble with daily activities (like writing, dressing, or walking)
One key symptom they look for is bradykinesia, which means slowness of movement. It can show up as:
- A reduced arm swing while walking
- Difficulty getting out of a chair
- Taking more time to button clothes or perform small tasks
To confirm Parkinson’s, the doctor also checks for at least one of these:
- A resting tremor (shaking, usually when the body is relaxed)
- Muscle stiffness
- Balance issues not caused by vision or inner ear problems
What Strengthens the Diagnosis?
Doctors feel more confident it’s Parkinson’s if:
- Symptoms started on one side of the body and gradually worsened
- There’s a good response to Parkinson’s medications, like levodopa
- A resting tremor is present
- The person has non-motor symptoms, such as:
- Loss of smell
- Constipation
- Sleep disturbances (like REM Sleep Behavior Disorder)
- Mood changes or memory issues
They also rule out other possible causes, such as side effects from medication, strokes, or other neurological disorders.
Can Tests Help? Yes — But They’re Not Always Needed
Though tests don’t “prove” Parkinson’s, they’re often used to rule out other conditions or to support the diagnosis when symptoms aren’t typical.
1. MRI Brain
An MRI helps rule out other causes like stroke, brain tumor, or fluid buildup that could mimic Parkinson-like symptoms.
2. DAT Scan or F-DOPA PET Scan
These imaging tests show dopamine activity in the brain. Since Parkinson’s causes reduced dopamine, these scans can help differentiate Parkinson’s from other movement disorders, such as essential tremor.
3. FDG PET Scan (Glucose PET)
This test looks at how the brain uses glucose (its energy source). In Parkinson’s, specific brain regions show a unique pattern of reduced activity.
It’s especially helpful when:
- The symptoms are unusual
- Doctors are considering atypical Parkinsonism (like PSP or MSA)
- There’s a need to distinguish from other conditions like Alzheimer’s disease
FDG PET isn’t done in every case, but it can offer valuable insights when the diagnosis is unclear.
Final Thoughts: Diagnosing Parkinson’s Is a Journey
Parkinson’s Disease is diagnosed through careful observation, clinical experience, and, when needed, supportive testing. It’s not just about what shows up in scans, but how you move, feel, and function over time.
If you or a loved one is experiencing symptoms like slowness, tremors, or balance issues, don’t ignore them. Early diagnosis and treatment can make a meaningful difference in managing Parkinson’s and maintaining quality of life.
When in doubt, talk to a neurologist — because every step counts.