Written By Aisha , Reviewed by Dr. Manvir Bhatia-6/02/2026
Sleep is not just about rest — it is deeply connected to hormones, especially in women. From puberty to menopause and beyond, hormonal changes continuously influence how women fall asleep, stay asleep, and feel after waking up. Understanding this connection helps women recognize what is normal, what is not, and how to manage sleep-related challenges effectively.
This blog explains how hormonal changes begin, why they affect sleep, how problems develop, how to control negative effects, and how women can monitor their sleep health at every stage of life.
1. The Hormone – Sleep Connection: “Why It Matters”
Hormones act as chemical messengers that regulate many body functions, including:
- Sleep–wake cycles
- Body temperature
- Mood and stress response
- Metabolism and energy levels
Key hormones affecting women’s sleep include:
- Estrogen – Estrogen helps regulate neurotransmitters involved in sleep and mood. Balanced estrogen levels support deeper sleep and healthy REM cycles, while low levels can cause fragmented sleep and frequent awakenings.
- Progesterone – Progesterone has a natural sedative effect by enhancing GABA activity in the brain. This helps reduce anxiety, promotes relaxation, and makes it easier to fall and stay asleep.
- Melatonin – Melatonin is released in response to darkness and signals the body that it is time to sleep. Disruption in melatonin secretion can lead to delayed sleep onset, insomnia, or irregular sleep-wake cycles.
- Cortisol – Cortisol normally decreases at night, allowing sleep to occur. Elevated nighttime cortisol due to stress can cause difficulty falling asleep, light sleep, or early morning awakenings.
- Thyroid hormones – Thyroid hormones regulate energy levels and brain activity. Excess levels can cause restlessness and insomnia, while low levels may lead to excessive sleepiness and fatigue.
When these hormones fluctuate, sleep patterns often change.
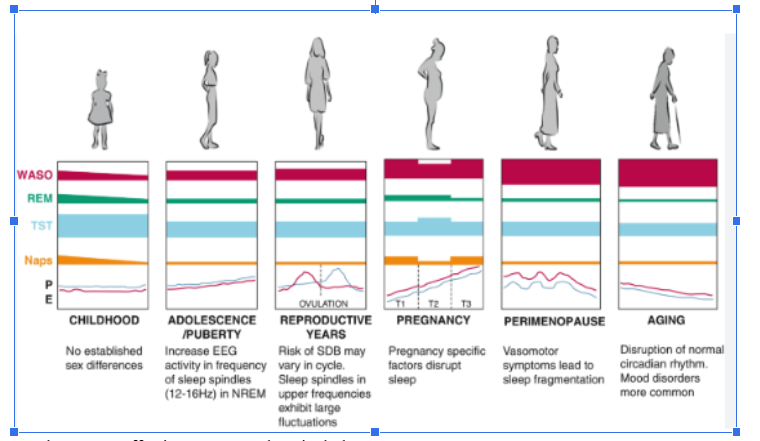
2. Childhood & Puberty: “When Changes Begin”
How It Starts: During puberty, estrogen and progesterone levels begin to rise. At the same time, melatonin release shifts later at night.
How It Impacts Sleep
- Difficulty falling asleep early
- Irregular sleep schedules
- Increased daytime sleepiness
- Emotional sensitivity affecting sleep quality
Why It Happens: The body clock (circadian rhythm) shifts naturally during adolescence, while hormonal surges affect mood and sleep regulation.
How We Control:
- Consistent sleep and wake times
- Limiting screen use before bedtime
- Educating young girls about sleep changes
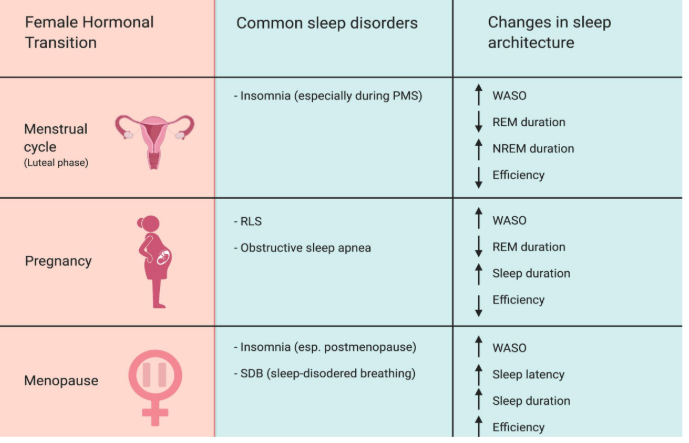
3. Menstrual Cycle: “Monthly Sleep Fluctuations”
Many women notice that their sleep changes throughout the month—and it’s not “just in your head.” Hormonal shifts during the menstrual cycle directly affect sleep quality, energy levels, and even dreams. Understanding these phases can help you be kinder to your body and plan better rest.
Key Phases & Their Effects
- Menstrual Phase (Days 1–5)
Sleep may feel lighter or restless due to cramps, discomfort, or low estrogen. Fatigue is common, so extra rest and gentle routines help. - Follicular Phase (Days 6–13)
Rising estrogen improves mood and sleep quality. Many women feel more refreshed, focused, and energized during this phase. - Ovulation (Around Day 14)
Sleep is usually stable, but some may notice slightly lighter sleep or vivid dreams as body temperature increases. - Luteal Phase (Days 15–28)
Progesterone initially promotes sleep, but closer to the period, hormonal drops can cause insomnia, night awakenings, or PMS-related sleep issues.
Why It Happens: Progesterone initially promotes sleep, but its sudden drop before menstruation disrupts sleep stability and mood.
How to Control It
- Maintain regular bedtime routines
- Reduce caffeine and salty foods before periods
- Practice relaxation techniques
4. Pregnancy: Sleep under Constant Hormonal Change
Pregnancy is a beautiful phase of life, but for many women, it also brings restless and interrupted sleep. From the first trimester itself, rising hormones begin to change how the body rests. These hormonal shifts are essential for supporting the baby’s growth, yet they can affect comfort, breathing, and normal sleep rhythms.
How Hormones Affect Sleep
During pregnancy, key hormones play a major role in sleep changes. Progesterone increases sleepiness, especially early on, but can also cause frequent nighttime awakenings. Estrogen affects nasal passages and circulation, often leading to congestion, mouth breathing, and vivid dreams. At the same time, rising cortisol levels increase nighttime alertness, making sleep lighter and less continuous.
Common Sleep Issues
As the body adapts, many women experience:
- Frequent nighttime urination
- Heartburn and breathing discomfort when lying down
- Restless, light sleep with vivid dreams
Why It Happens & What Helps
These changes occur because pregnancy hormones reshape breathing, circulation, metabolism, and sleep architecture in preparation for childbirth. Simple habits can help improve rest:
- Sleep on the left side for better blood flow
- Eat small, frequent meals to reduce heartburn
- Take short, early naps if needed
- Seek medical advice if snoring or breathing problems appear
5. Postpartum Period: Sleep Deprivation & Hormonal Drop
The weeks after childbirth are joyful, emotional, and deeply exhausting. During the postpartum period, a mother’s body undergoes a sudden hormonal shift while adjusting to the constant demands of newborn care. This combination often leads to significant sleep disruption, both physically and emotionally.
What Changes After Delivery
After childbirth, hormone levels change rapidly:
- Estrogen and progesterone drop sharply, affecting mood regulation and sleep stability
- Prolactin levels increase to support milk production, which can alter normal sleep–wake rhythms
How Sleep Is Affected
- Difficulty falling or staying asleep, even when the baby is resting
- Emotional exhaustion, mood swings, and increased sensitivity
- Higher risk of postpartum insomnia or depression, especially when sleep loss
Why It Happens: Sudden hormonal withdrawal, combined with nighttime feeding, irregular sleep schedules, and physical recovery, disrupts the body’s natural sleep architecture. The brain remains on “high alert,” making restorative sleep harder to achieve.
Precautions & When to Seek Help
- Sleep when the baby sleeps
- Share nighttime responsibilities
- Seek help if insomnia persists beyond a few weeks // visit to sleep specialist doctor.
6. Perimenopause & Menopause: “Major Sleep Disruptors”
For many women, perimenopause and menopause mark a time when sleep suddenly becomes difficult. Nights that were once restful may turn into hours of tossing, waking, and early morning alertness. These changes are closely linked to shifting hormone levels and how they affect the brain and body.
Hormonal Changes Behind Sleep Disturbance
During this phase, estrogen and progesterone levels gradually decline, removing their natural calming and sleep-supporting effects. At the same time, melatonin production becomes irregular, disrupting the body’s internal clock and making it harder to fall and stay asleep.
Sleep Problems Commonly Seen
- Hot flashes and night sweats that cause sudden awakenings
- Frequent nighttime awakenings with difficulty returning to sleep
- Early morning awakening, even after short sleep duration
- A higher risk of chronic insomnia, especially when stress or anxiety is present
Why Sleep Gets Worse: Estrogen plays a key role in regulating body temperature, mood, and sleep stability. As estrogen declines, the body becomes more sensitive to temperature changes, its decline leads to thermal discomfort and anxiety, disrupting sleep.
How to Manage
- Maintain a cool, well-ventilated sleeping environment
- Follow fixed sleep–wake schedules to support circadian rhythm
- Seek medical consultation for severe or persistent symptoms
- Consider Cognitive Behavioral Therapy for Insomnia (CBT-I), a proven non-medication treatment
7. Post-Menopause & Aging: Sleep Quality Over Quantity
As women move through post-menopause and into later adulthood, sleep often changes in noticeable ways. While total sleep hours may reduce, the bigger shift is in sleep quality. Many women find that they sleep lighter, wake up more often, and feel less refreshed — even after spending enough time in bed.
What Happens to Sleep?
With aging and hormonal changes, the natural sleep rhythm becomes more fragile:
- More frequent awakenings during the night
- Lighter sleep, with less deep and restorative stages
- Earlier sleep and wake times, often feeling sleepy in the evening and waking up too early
These changes are common and not a sign of illness—but they can still affect daily energy and mood.
Contributing Factors
- Reduced melatonin production, making it harder to stay asleep through the night
- Other health conditions or medications, which may disturb sleep
- Increased sensitivity to stress, causing the mind to stay alert at night
Helpful Strategies for Better Sleep
- Daytime physical activity
- Exposure to morning sunlight
- Avoid long daytime naps
8. How Women Can Tell If Their Sleep Is Healthy or Not
Signs of Healthy Sleep
- Feeling refreshed on waking
- Stable mood and energy
- No excessive daytime sleepiness
Warning Signs of Poor Sleep
- Trouble falling asleep regularly
- Frequent night awakenings
- Daytime fatigue or headaches
- Mood swings or poor concentration
If symptoms persist for more than 2–3 weeks, professional sleep evaluation is recommended.
9. General Precautions for Women at All Ages
- Maintain consistent sleep schedules
- Limit caffeine after afternoon hours
- Avoid screens 1 hour before bed
- Practice stress management
- Track sleep changes with menstrual or life stages
- Seek medical advice rather than ignoring chronic sleep issues
Conclusion
Hormonal changes are a natural part of a woman’s life, but sleep disruption does not have to be. By understanding how hormones affect sleep at each stage, women can take informed steps to protect their sleep health, recognize warning signs early, and seek timely support.
Good sleep is not a luxury — it is a foundation for physical, emotional and hormonal well-being for every age group women’s.