Obstructive Sleep Apnea Treatment
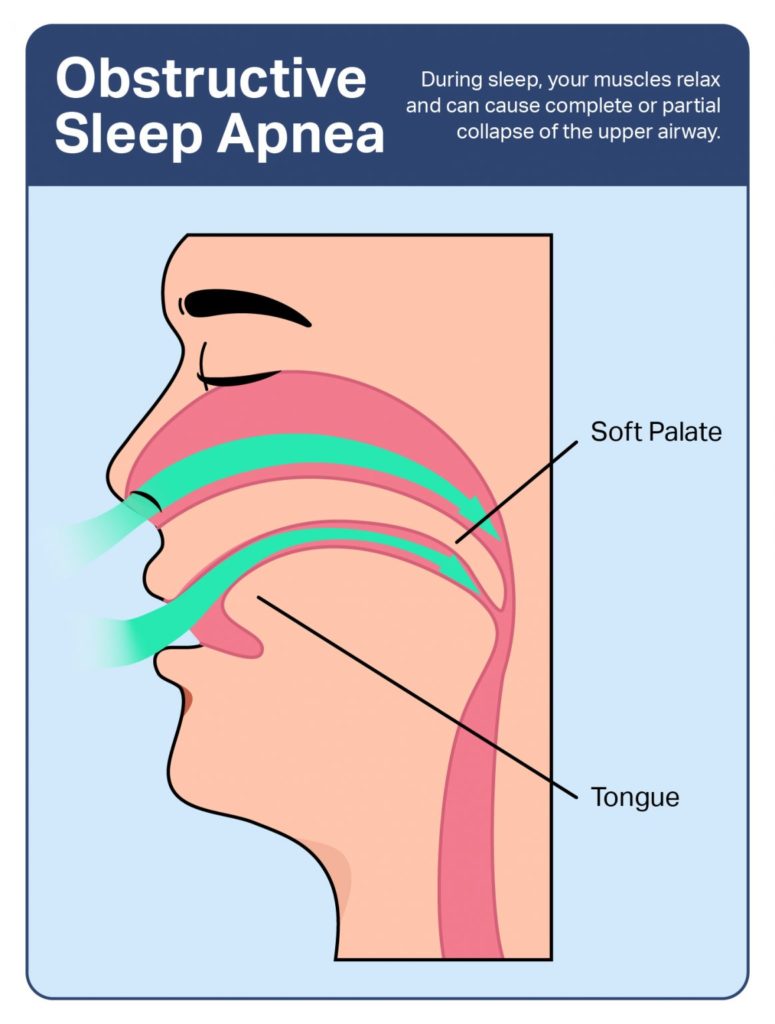
Obstructive Sleep Apnea (OSA) is a condition that causes a person’s airway to become partially or completely obstructed during sleep, resulting in interrupted breathing. This can lead to a decrease in oxygen levels in the blood, which may trigger the brain to briefly wake the person to restore normal breathing. These interruptions in sleep can occur hundreds of times a night, disrupting the quality of sleep and leading to various health issues.
Key Details about OSA::1. Causes of OSA:
OSA occurs when the muscles in the back of the throat relax excessively during sleep. This causes a temporary blockage of the upper airway, which can prevent proper airflow to the lungs. Common causes of airway obstruction include:
2. Risk Factors for OSA:
Several factors increase the likelihood of developing obstructive sleep apnea, including:
3. Symptoms of OSA:
The symptoms of obstructive sleep apnea can vary, but the most common signs include:
4. Diagnosis of OSA:
OSA is typically diagnosed through a combination of medical history, symptoms, and sleep studies. Common methods of diagnosis include:
5. Health Risks of Untreated OSA:
If left untreated, OSA can contribute to a variety of serious health complications, such as:
6. Treatment Options for OSA:
Treatment for obstructive sleep apnea aims to alleviate symptoms, improve sleep quality, and reduce the associated risks. Treatment options include:
Continuous Positive Airway Pressure (CPAP): This is the most common treatment for moderate to severe OSA. A CPAP machine delivers a constant stream of air through a mask that keeps the airway open during sleep.
Bilevel Positive Airway Pressure (BiPAP): Similar to CPAP, but it delivers two levels of pressure (one for inhalation and one for exhalation). This is often used for people who cannot tolerate CPAP.
Oral appliances:These are devices that help reposition the lower jaw and tongue to keep the airway open. They are typically used for mild to moderate cases of OSA.
Surgery:
- Tonsillectomy or adenoidectomy: Removal of the tonsils or adenoids if they are causing airway obstruction.
- Uvulopalatopharyngoplasty (UPPP): Surgical removal of excess tissue in the throat to enlarge the airway.
- Genioglossus advancement (GA): Surgery to reposition the muscle that controls the tongue.
- Maxillomandibular advancement (MMA): Surgery that repositions the upper and lower jaw to increase airway size.
- Inspire therapy: A surgically implanted device that stimulates the airway muscles to keep the airway open during sleep.
- Medications: There are no specific medications to treat OSA, but sometimes medications may be prescribed to address related conditions such as high blood pressure, depression, or sleepiness.
7. Managing OSA Long-Term:
In addition to the above treatments, long-term management of OSA often includes regular follow-up with a healthcare provider to monitor treatment effectiveness. Consistent use of CPAP or BiPAP devices is essential for people with moderate to severe OSA, and the use of oral appliances may require periodic adjustments. Lifestyle changes should be maintained, and a person with OSA should work with their healthcare provider to ensure that their condition is being properly managed.
If you have specific concerns about OSA, such as treatment options, or if you're considering getting tested, it's always a good idea to consult with a sleep specialist or doctor to discuss your symptoms and best course of action.

